SKINIAL is a pioneer and the only company in the world that has been exclusively researching cosmetic tattoo removal. We draw our knowledge from scientific findings and from our practical experience since 2009 in 20 countries with hundreds of studios and over 80,000 treatments to date.
Structure
- Preliminary remark
- Scars and other side effects of tattoo removal
- The causes of tattoo removal scars
- What the client can do to avoid scarring
- What are the treatment options for scars after tattoo removal?
Preliminary remark
Almost every tattoo and every tattoo or PMU removal leaves scars. Some are visible to the naked eye and can be felt with the fingers (cosmetic definition). Others can only be seen under a microscope (dermatological definition).
While some clients are mainly concerned with the pigmentation no longer being visible, others expect that after the treatment, the skin will be restored to look as it did before the pigmentation. In many cases, the perfect result is even quite close, in most cases it succeeds more or less well and in rare cases side effects show up, which also include scars.
Without question, every visible scar that appears after a treatment is one too many. In an explanatory talk that precedes every treatment, the client is explained in detail which reactions of the skin are possible and which side effects can occur.
Nevertheless, visible scars are merely aesthetically undesirable, but not problematic for health or life. They are a natural individual reaction of the immune system to external aggression. What triggered the scarring can be easily determined in most cases. The actual causes for the appearance of scars can rarely be determined with certainty.
Scars and other side effects of tattoo removal
Our explanations do not claim to be medically or scientifically complete but are merely intended to provide a good overview for the interested layperson. We mention medical terms only where necessary and translate them into colloquial terms. However, some medical terms have already found their way into colloquial language.
Scars
Below we list the most common scars in alphabetical order.
Burn scars
Burns only occur with laser treatments, not with cosmetic methods. The known cosmetic removal products are applied in concentrations that cannot cause burns. Laser treatments, on the other hand, generate temperatures of up to 900°C, which can lead at least to painful burns in the dermis but also in the epidermis if the treatment is not carried out properly, e.g., unsuitable frequency selection of the laser head. This should not happen if the laser is used as intended. Nevertheless, the use of laser devices is almost always very painful.
Photo SKINIAL (skin burns after laser treatment)

Hypertrophic scars (bulge scars)
They usually develop 4 – 8 weeks after the irritation caused by the treatment, after or during wound healing. The growth phase lasts 1-6 months. Hypertrophic scars regress in 90% of all cases. In some cases, this can take up to two years. We have observed an increased risk in regions with high UV exposure and high humidity (e.g., tropics).
Source: SKINIAL
Source: Canva


Keloids
A special form of hypertrophic scar is the keloid. It is not limited to the treatment site but proliferates beyond the treatment site. Some parts of the body are genetically particularly susceptible to keloids (upper chest and upper neck).
According to several medical studies*, the development of a keloid has genetic causes in more than 50% of cases. Therefore, keloids are recognised as a skin disease. In dark-skinned people, the occurrence is more frequent and possible completely without cause.
Keloids are very persistent. The perspective of regression is significantly worse compared to hypertrophic scars, although not impossible. However, surgical removals often lead to the keloids reappearing (recurrence).


SKINIAL: Keloid before treatment with toxic pigments
SKINIAL: Classic keloid
Sclerotic scars (shrinkage scars)

Other side effects
Apart from scars, the side effects are temporary and largely negligible, except perhaps for burn blisters, which however can only be caused by the high heat during laser treatments.
Redness
Most common side effect, which is due to increased blood supply to the capillaries (fine blood vessels in the upper part of the dermis down to the epidermis) to speed up healing. Lightening and complete disappearance in almost all cases. The longer the redness persists, the worse the individual wound healing.
Itch
Often a side effect of scarring, but also of allergic reactions due to toxic pigment components.
Pain
Occur with infections or when sclerotic scars restrict freedom of movement. They are usually temporary phenomena.
The causes of tattoo removal scars?
Pigments – the culprits
For the body, introducing artificial pigments into the skin is comparable to penetrating dirt. Under normal circumstances, an infection with subsequent rejection would occur immediately. To prevent this, the macrophages encapsulate the large piles of pigment so that they become invisible to the immune system. In this way, they can remain unnoticed in the skin for decades. Small pigment particles are immediately transported via the lymphatic system to the lymph nodes where they are finally deposited. Very small pigment particles in the nano range can also enter the bloodstream and even the brain. The more pigment colour is deposited in the lymph nodes, the greater the risk of disorders caused by immune reactions.
The body already produces antibodies on first contact, which can take up to three weeks depending on the substance. By then, the pigments are usually no longer visible to the immune system, so allergic reactions rarely occur during the pigmentation itself. Unfortunately, there are hardly any long-term studies on this, but increasing numbers of allergies and general clinical pictures without obvious causes are constantly on the rise. The “pollution” of the immune system is increasingly suspected as a cause, which can lead to false alarms and disturbances of the system. Every side effect you perceive is triggered by the immune system.
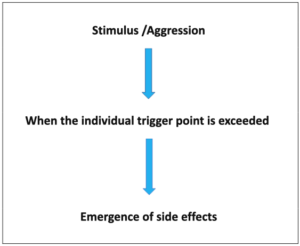
The path from treatment to side effect
Basically, side effects are protective mechanisms of the body against externally perceived aggression. It can also be seen as a cry for help from the body, which wants to protect the “attacked” treatment site through various measures. Medical literature often speaks of the “overreaction of the immune system” when side effects are triggered even by minor irritation.
Only when the individual stimulus threshold of the human being is exceeded does a reaction of the immune system occur, which manifests itself through the formation of side effects.
What are the most common side effects?
The most common side effects of removal are redness, itching or temporary pain, or burn blisters from the laser, but these usually subside after a short time. Contamination of the treatment site by dirt infections (bacteria and viruses) prolongs the healing process. They are avoidable and should quickly fight and reduce the infections if suitable products are used (e.g., MEDICLEAN by SKINIAL).
Due to the release of the colour molecules during removal, even the smallest traces of toxic components in the pigments can trigger immune reactions that can lead to allergic reactions. Since the original pigmentation, the immune system has created antibodies that are present in your blood and are immediately activated upon contact with the toxic molecules. This explains why immune reactions are often even more severe on second contact with the skin. These allergic reactions can lead to itching and pain and in rare cases to more severe reactions, up to the dangerous nickel allergy or an extremely rare hyperglycaemic shock.
UV radiation during regeneration of the still young skin at the treatment site can trigger severe immune reactions. The same applies to friction, pressure, and moisture before or shortly after wound closure following treatment. Smoking, alcohol, stress, drugs, or vigorous exercise also delay wound healing and can trigger immune reactions.
How a scar develops
The formation of a scar occurs through excessive production of collagen tissue. This creates a dense barrier that protects but is aesthetically undesirable. This protective layer is not normal, healthy skin that contains hair or glands. The elevation of the skin at the treated skin sites is called “hypertrophic scars” (see also sub-1. above). In 90% of cases, the immune system regresses hypertrophic scars when the immune system decides that it does not (no longer) need the scars for protection. Every year, more than 500 million hypertrophic scars develop and regress, mainly after surgery.
If the scar grows beyond the treatment sites, it is a keloid (see also above under 1). If skin openings (wounds) are too large, if the treated areas are not sufficiently protected during wound healing (friction, active sports, UV radiation, constant movement), the wound heals poorly together and sclerotic scars develop (see also above under 1).
How likely is the occurrence of scars?
No one can predict with certainty whether side effects will occur during or after treatment and when the immune system will overreact. This depends too much on the circumstances of the treatment, the genetic predisposition, and the general state of health of the client. Furthermore, it also plays a role whether the skin is young or old, sensitive, or rather resistant, whether it has had previous damage and much more.
The toxic substances mentioned above as triggers of immune reactions are still little known and researched. In “every” pigment colour, even in organic colours, there are minute, often merely molecular, traces of toxic substances that can trigger allergic reactions of the immune system. Whether a reaction is triggered is by no means certain. This is due to the individual and constantly fluctuating stimulus threshold of the human being. Depending on the strength of the immune system, it reacts sometimes more strongly sometimes weakly. Thus, one and the same person can have a reaction today and nothing happen the next day to the same stimulus. Also, some parts of the body may be affected, sometimes only partially. What, when and where happens remains the great secret of our immune system.
Although there are higher legal limits for pigments every few years, these are set by commissions. The result is always a compromise of the interests of industry and medicine. This does not mean that even significantly lower amounts can cause severe reactions in some people. Otherwise, the limits would not be regularly adjusted upwards.
Of course, the method used, the compliance with legal regulations and especially the professionalism (training and experience) of the user play an important role, as well as the aftercare and hygiene by the client. All these framework conditions have an influence on the occurrence of possible side effects and their manifestation.

The connection between treatment (triggers) and the causes of scars
A correlation between scar and tattoo removal treatment is often obvious, but it is difficult to provide sufficient proof of the actual cause. Therefore, one can only very rarely conclude causality from a correlation. It is therefore practically impossible to name with certainty a specific cause for the occurrence of side effects, or equally impossible to exclude a specific cause.
The attempts of some experts, but also of ill-informed lay people, to locate a method, a product or even a company as the cause for the occurrence of side effects, especially scars, therefore come to nothing in most cases.
Beware of first impressions. The actual reasons are often more diverse and not obvious at first sight

What the client can do to avoid scarring
Many clients underestimate their own contribution to the regeneration and healing of the treatment site.
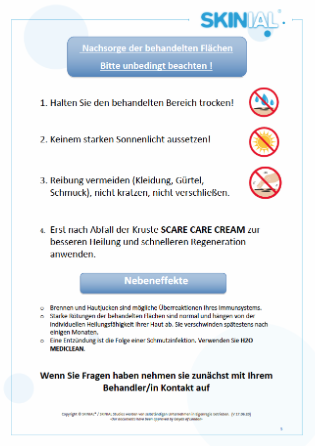
Whether a scar develops is largely determined by the aftercare. The treatment site (epidermis) generally heals without scars if cosmetic treatment has been carried out. The process of wound healing is genetically determined, but it can be hindered by many factors, which can promote poor healing and scars.
- Strong movements of the treated area are often unavoidable, but can delay healing (fingers, wrist, …).
- Infections are caused by dirt that gets into the wound from the outside and which then impedes the healing process, which can lead to sclerotic scars, for example (the wound grows together incorrectly, bulges form).
- Intense sports, friction from clothing, UV radiation, humidity and moisture can also lead to problems with wound healing.
- Treat the treatment area with a suitable ointment (SKINIAL recommends: SCAR CARE CREAM) as soon as the wound is closed, and the scab has fallen off.
The customer receives this information sheet after each treatment
What are the treatment options for scars after tattoo removal?
Many cosmeticians have specialised in scar treatment and achieve amazing results with different methods, even with surgical scars. A detailed description would go beyond the scope of this presentation. But doctors also treat scars with different methods. The boundaries between medical and cosmetic methods are fluid.
Medical methods, e.g., surgical methods, cold methods (cryo-therapy) or laser methods, may only be performed by doctors; this is not allowed for cosmeticians in Europe. However, this does not automatically mean that medical treatments always produce better results.
It is often possible for the affected person to achieve significant improvements in the appearance of the skin with simple means. An efficient method is to massage the raised scars several times a day for a few minutes with gentle pressure. Use a little oil so that there is less friction but more pressure on the area. This promotes blood circulation, loosens the tissue and signals to the immune system that the excess collagen is not needed, which often leads to regression.
Dr. Sanchez, a doctor and trainer practising in Madrid, achieves success in the regression of hypertrophic scars and keloids by lowering the individual’s overall stimulus level. A healthy lifestyle and more rest play a decisive role in this.

